Diabetes Mellitus (diabetes) is a disease or condition that occurs in both young and old. In diabetes, the balance in blood sugar levels is disrupted because the pancreas produces insufficient insulin.
Insulin ensures that the muscles and other organs can use the energy in the diet. If there is too little insulin, the body cells cannot use the fuel they need. There will then be too much sugar in the bloodstream, causing the blood sugar level to rise.
A large part of the patients who are being treated by the podiatrist have foot complaints as a result of diabetes. These are mainly people who have been diabetic for a longer period of time. Almost 50% of this group will develop foot complaints as a result of their diabetes in the long term. In the long term, the interaction of deteriorating blood circulation (angiopathy) of the foot in combination with the poorer functioning of the nervous system (neuropathy) will be the cause of the development of the diabetic foot.
As one suffers from diabetes mellitus for a longer period of time, characteristic complications occur:
- Angiopathy; vascular abnormalities that lead to narrowing of the blood vessels, which impairs the blood flow to tissues and organs. As a result of the reduced blood supply, the risk of infections will increase and a wound will heal less quickly. In a severe case, this can lead to the loss of toes or part of the foot.
- Neuropathy; complications to the nerve pathways, where the sense of feeling decreases, especially in the feet and lower legs. One often has a numb feeling in the feet (feeling like walking on cotton wool). A wound can also be less quickly noticed because it cannot be perceived in time. One does not feel pain. One gets a dry thin skin due to the reduced functioning of the sweat glands. This can also cause wounds to occur earlier. If the nerves in the foot are affected, an abnormal foot position or unstable walking pattern can occur. The chance of pressure spots
/complaints on the toes, under the foot, heel and ankle increases.
- Ulceration (wound formation); is common in the diabetic foot and must be treated and seen accurately by a podiatrist to prevent amputations. Ill-fitting shoes, but even seams of socks can create wounds that are not well felt by someone whose superficial feeling is reduced. A podiatrist can inform you about how to prevent wounds and how they should be treated.
Because Diabetes Mellitus is a systemic disease that affects multiple parts of the body, a multidisciplinary approach is necessary. To achieve prevention, early recognition of risk factors and regular foot screenings are necessary.
In addition to these screenings, which include checking the sense of feeling and blood flow in the feet, but also looking at (future) risks for complications, the podiatric possibilities consist of:
- Instrumental treatment in which excessive calluses are removed
- Instrumental wound treatment
- An orthosis to relieve pressure points/corns or to correct/compensate for a deviating toe position
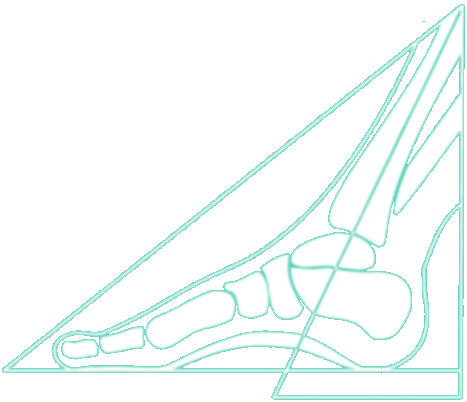
- Therapeutic insoles to relieve pressure points or to correct/compensate for a deviating foot position
- Wash your feet daily with lukewarm water. Dry them gently with a soft towel and especially between and under the toes. If there is too little space between the toes or if the toes are difficult to separate, use a tea towel. If the skin is too dry, use a good foot cream, but do not apply it between the toes.
- Inspect your feet every day to detect 'foreign' spots. Think of cracks, wounds, cracks, blisters, discoloration of the skin (blue, redness) or changes in the toenails. Use a mirror to look under the foot and between the toes. If someone cannot view their feet themselves due to poor eyesight, ask your partner, family or friends. It is important.
- Inspect the shoes before putting them on by feeling with your hand if there is anything in them (such as stones).
- Never walk barefoot, not even at home. Then walk on slippers or slippers.
- Avoid tight socks and tights with seams. These can damage the skin and impede blood circulation.
- Cut nails straight. Never cut off the corners, as this can cause ingrown nails. If the toes are painful or the nails are too hard to cut yourself, visit a pedicure (with a diabetes note) or ask your podiatrist for advice.
- Never remove your calluses, warts, corns/corns yourself. Also do not use corn plasters, these can burn and damage the skin.
- Never take a foot bath longer than five minutes, otherwise the skin will become too soft and extra vulnerable to wounds and infection. Always rinse your feet with clean water. Do not take a foot bath with wounds.
- Always test the water temperature with your elbow. Due to nerve damage, it is possible that you do not feel that the water is too hot, which can cause burns.
- Do not walk on hot surfaces such as a sandy beach or tiles.
- Regular screenings are important. The podiatrist, but also the doctor's assistant/nurse can test your feet for
feeling (sensitivity) and blood flow.
- Make sure your feet are properly measured every time you buy new shoes. Ill-fitting shoes can be fatal for someone with Diabetes. Buy shoes later in the day, the feet are then 'larger' than in the morning. Pay particular attention to seams and seams at the toes and any bumps on the feet. Shoes should fit well immediately and 'breaking in' should not be necessary.
- Stop smoking! Smoking can adversely affect blood circulation. Which can already be a complication for people with Diabetes.